More and more workers compensation payers are recognizing the value of having direct agreements with strategic providers. Unfortunately, there are no options available to manage these agreements.
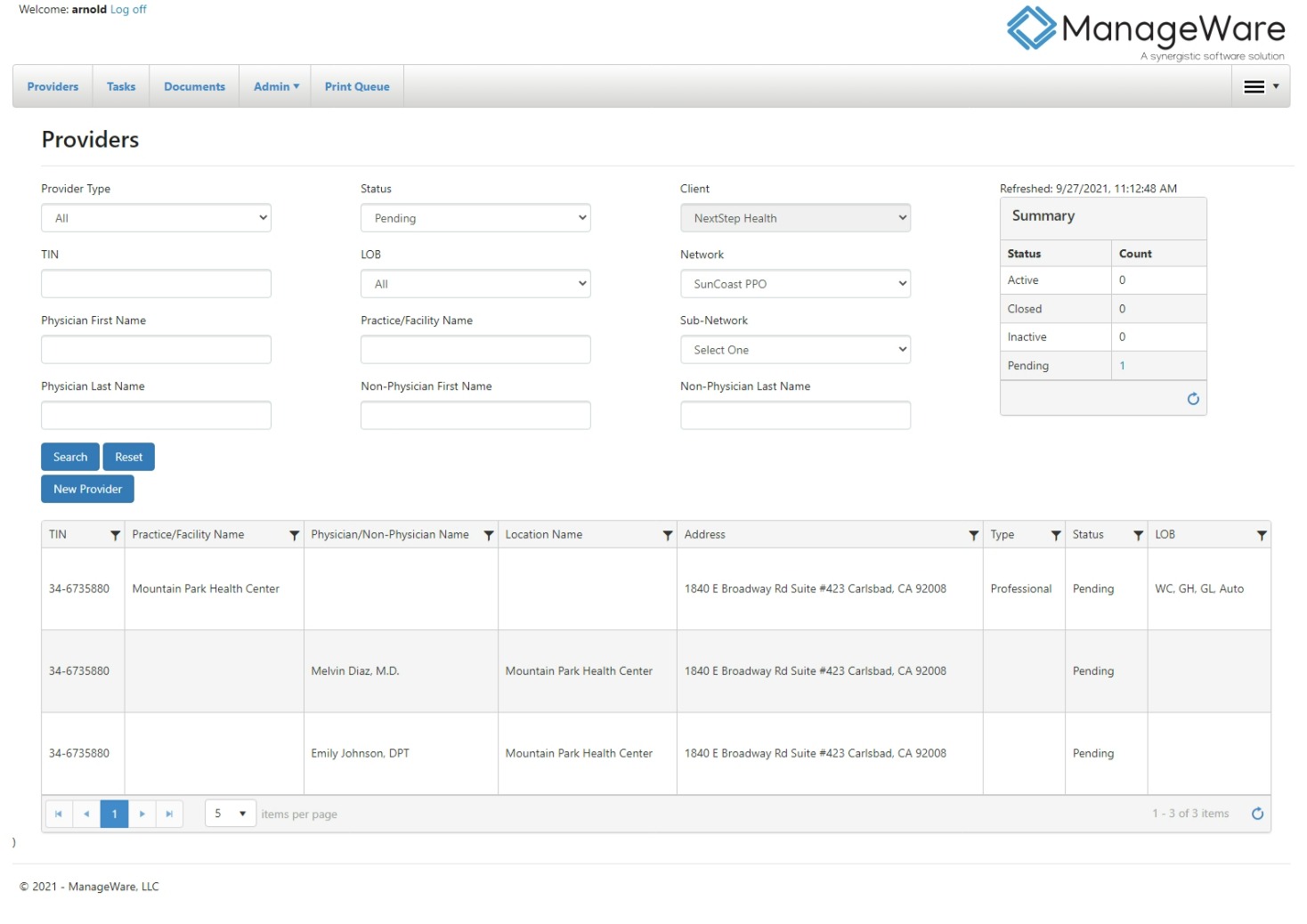
Now for the first time, ManageWare is offering NetworkManager, an independent provider network application. NetworkManager enables the simplification and enhancement of all provider network management activities. This robust, integrated workflow platform streamlines and organizes administrative tasks related to provider recruiting, credentialing, contracting and ongoing provider maintenance.
NetworkManager can also be fully integrated with MW Exchange, ManageWare’s provider portal, further streamlining the contract administration process. In addition, NetworkManager is fully integrated with ManageWare’s other managed care modules, or can interface with other independent third-party bill review platforms.
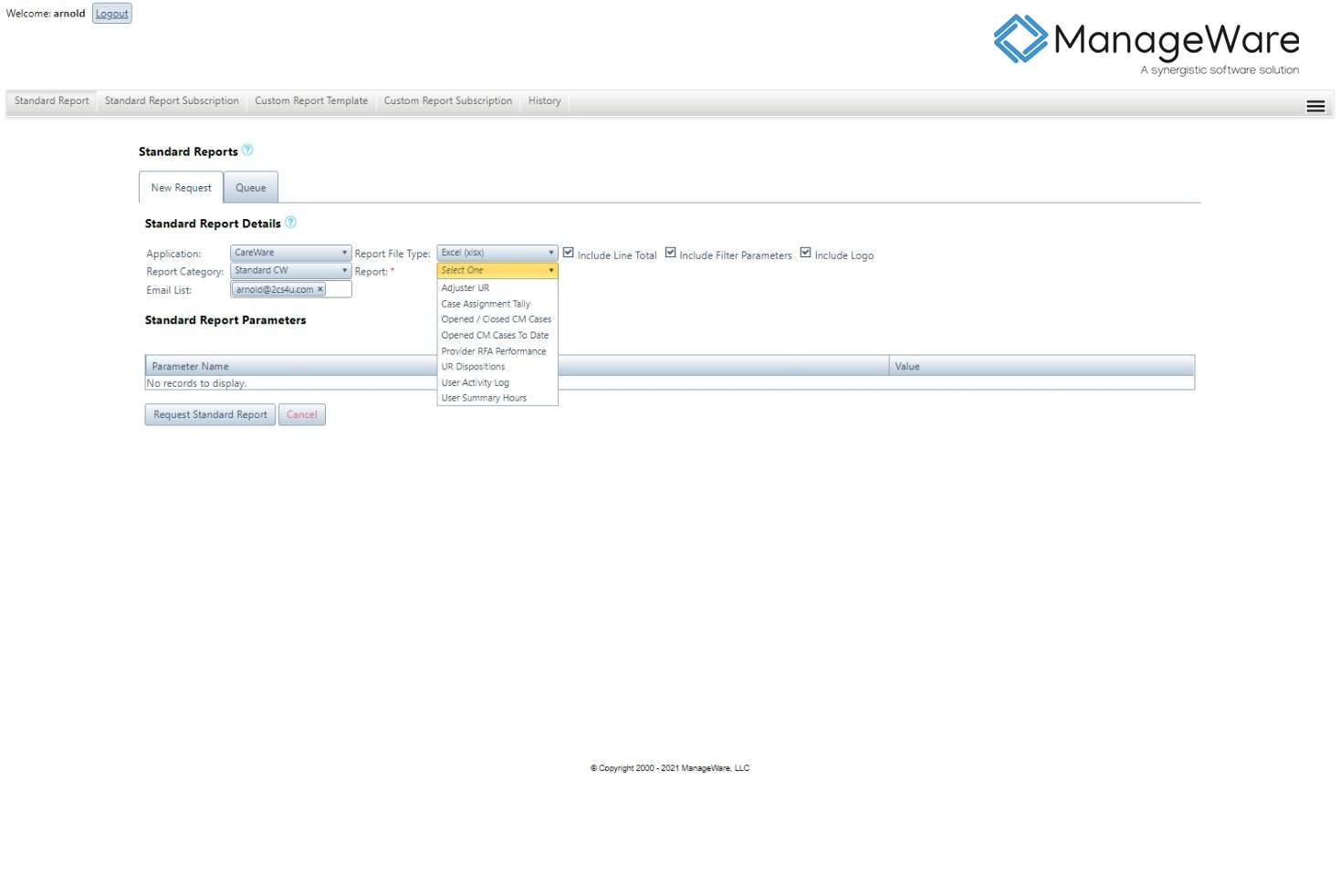
There is a full library of standard reports as well as a custom reporting capability available through our reporting module, ReportWare. Reports are set up on a subscription basis and generated on a preset schedule for distribution to the appropriate party. The subscription process is configured during implementation according to specific client requirements, and can be modified as necessary.