Most bill review companies claim to provide cost containment, but ManageWare goes beyond just medical saving to focus on the workflow and integration opportunities that add value and cost savings for our clients. ReviewWare is a proprietary web-based bill review platform that is fully integrated with all related processes and stakeholders in the medical management continuum, including utilization review, PPO networks, specialty networks, as well as treating providers.
The ReviewWare application can be accessed through our service bureau, where it is operated by our expert staff, or the software can be licensed and used by your staff if you manage your own internal bill review operation.
ManageWare offers a full-service outsourced bill review solution that integrates with multiple PPO and specialty networks. Our regulatory compliance department ensures bills are processed according to the correct and current fee schedules and offers multiple reporting capabilities including post-adjudication state reporting where required.


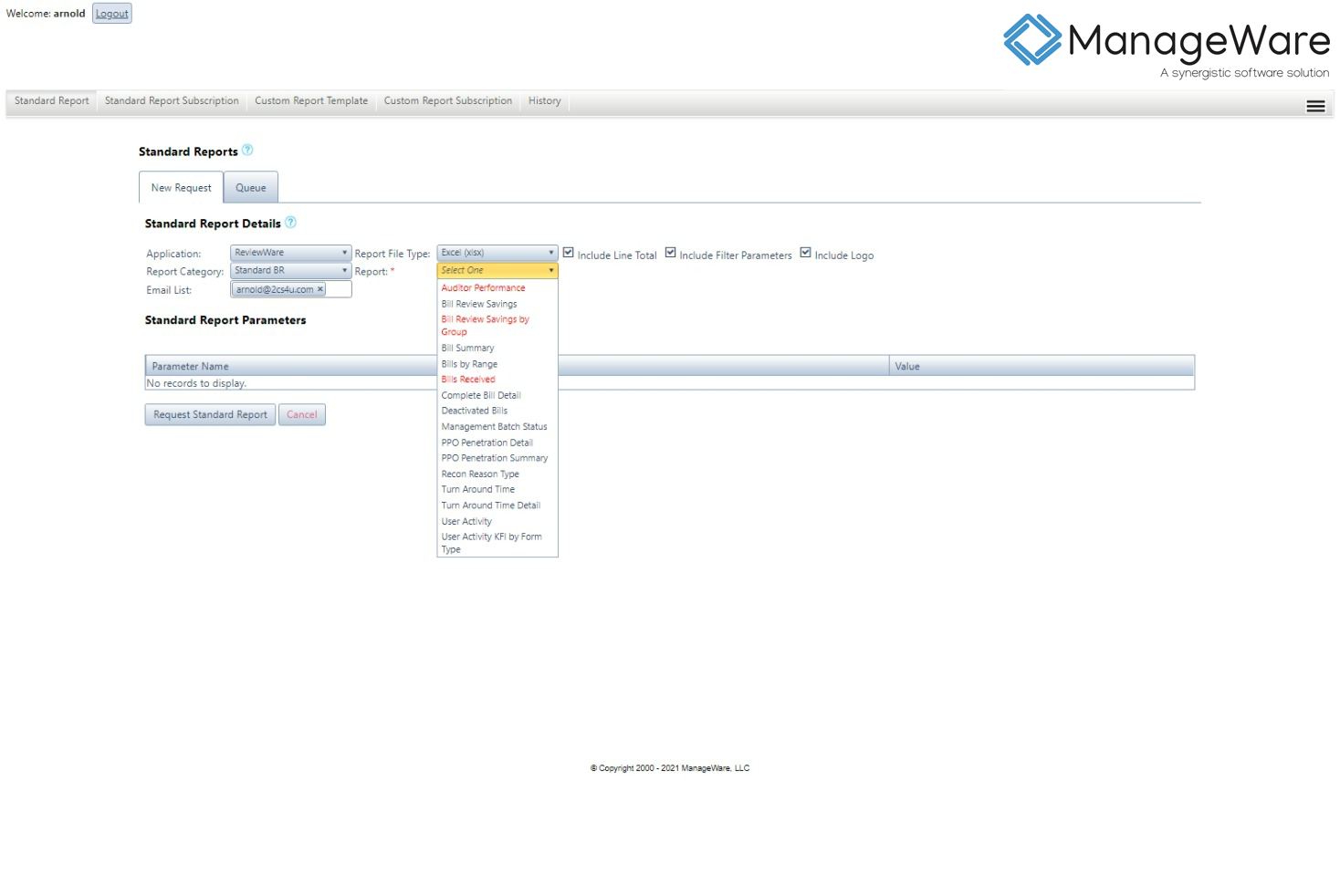
There is a full library of standard reports as well as a custom reporting capability available through our reporting module, ReportWare. Reports are set up on a subscription basis and generated on a preset schedule for distribution to the appropriate party. The subscription process is configured during implementation according to specific client requirements, and can be modified as necessary.